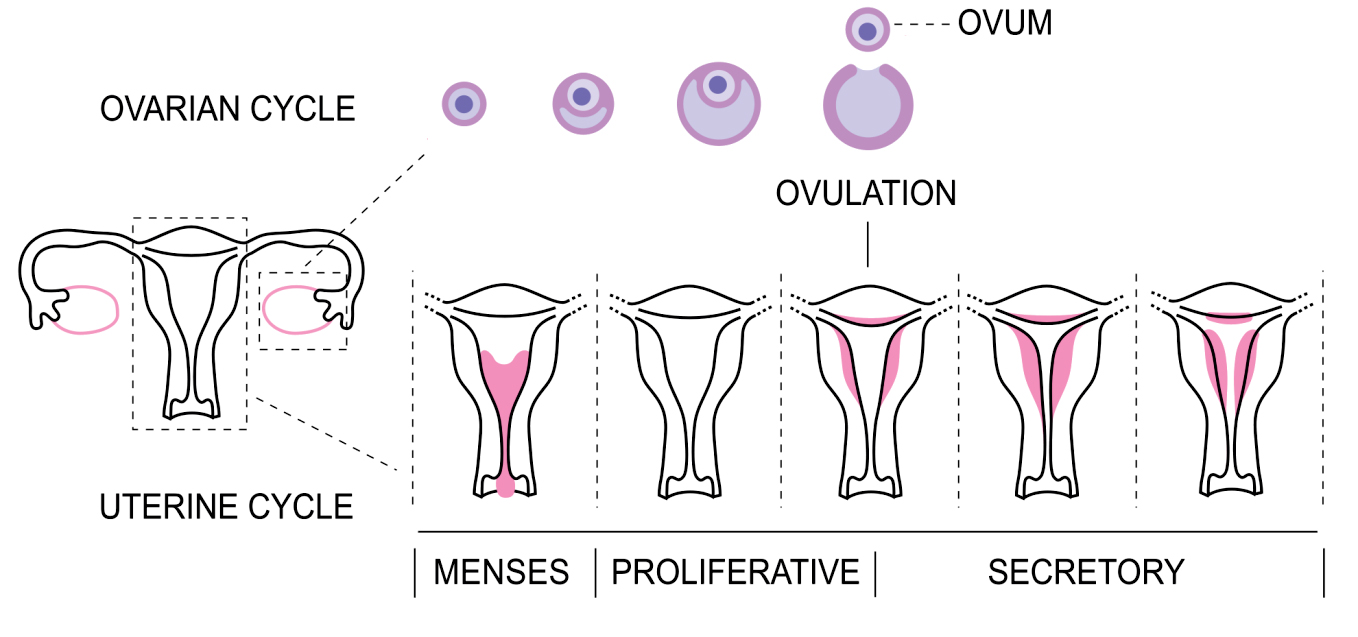
What is a normal menstrual cycle?
A normal menstrual cycle is a period every 28 days (21 – 35 days considered normal variant) with moderate bleeding for 3-7 days in a consistent pattern. A complex interplay of hormones results in ovulation which is the release of a single mature ovum every month. This is important to maintain regular menses and ensure fertility
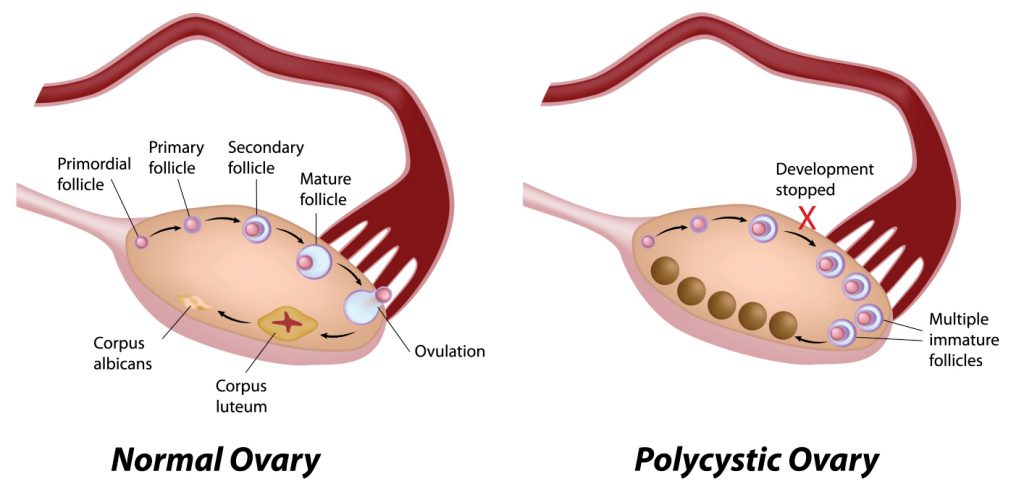
What is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder seen in 20-40% of women in the reproductive age group. A disturbance in the estrogen/ testosterone interaction in the ovary allows multiple ovarian follicles to grow every month but stops their maturation and ovulation. This leads to multiple, small, immature follicles (Polycystic ovaries). It is usually seen in overweight or obese girls/women but can occasionally also be detected in lean girls.
PCOS comprises of the following clinical features
- Irregular (delayed menses)
- Evidence of high testosterone (male hormone) activity: includes acne and excess body hair (hirsutism)
- Ultrasonography evidence of polycystic ovaries
PCOS is established if any 2 of the above criteria are met with exclusion of other conditions like hypothyroidism, prolactin excess, rare ovarian tumors and hormonal disorders.
When should you suspect PCOS?
The three main clinical features of PCOS are irregular menses,acne and excess facial and body hair (hirsutism). Menses delayed every cycle by more than a week happening from early teenage years should be evaluated for PCOS. These cycles usually get worse with weight gain. A recent change in menses in a lady who has always had regular cycles is unlikely to be PCOS. Acne (pimples) is also a manifestation and needs evaluation for PCOS. Excess body hair (hirsutism) in girls refers to thick hair in a male pattern distribution. These areas are face, chest, upper and lower abdomen and inner thighs. They may require frequent removal with threading,waxing or creams. Hirsutism usually worsens with age unless treated. PCOS is a spectrum with some girls having either acne or irregular menses or hirsutism whereas some have all three features.
How do we treat PCOS?
Weight reduction with healthy diet and regular exercises on accounting basis is very important. Treatment needs to be individualised depending on the clinical issues. Metformin is an insulin sensitizer and helps to control the metabolic issues and slowly improve the hormonal imbalance and regularize menses. It needs to be given with progesterone every 45-60 days to induce withdrawal bleed. It however works in only 50-60% of girls with PCOS, especially in those with a prediabetic state.
Hormonal contraceptives in the form of 21 day pills are the most effective to get regular menses and treat acne and hirsutism. However, the effects usually last till the medicines are on and may relapse once stopped. Anti androgen drugs like spironolactone, finasteride and flutamide are effective in hirsute girls.But they have to be stopped when pregnancy is planned. Topical creams for acne and facial hair can also be used in milder cases. LASER therapy is recommended for severe hirsutism. Girls with PCOS may need 8-12 LASER sessions depending on the severity.
Infertility is common in girls with PCOS. They may require ovulation inducing drugs like clomiphene citrate or hormonal injections for IVF. Metformin added to these drugs improves pregnancy chances and reduces risk of complications like ovarian hyperstimulation syndrome and GDM.
All girls with PCOS need to be monitored and treated for the metabolic problems like diabetes, hypertension, cholesterol and fatty liver disease.

Why is it important to Detect and treat PCO
- Risk of anovulation and infertility with irregular menses
- Cosmetic concerns with acne and hirsutism
- Metabolic concerns:increased risk of Gestational Diabetes Mellitus, type 2 diabetes, hypertension, high cholesterol, high uric acid, fatty liver disease and heart disease in later life.
Checklist for PCOS
FSH, LH, Thyroid profile, Prolactin, Testosterone, FBS, HbA1c, USG pelvis In special circumstances check for DHEAS,17(OH) progesterone, DHT, Cortisol,Growth Hormone.
Red herrings for PCOS
Delayed menses, acne, excess facial and body hair,male pattern balding,obesity,darkening of skin in neck folds,armpits and groins.
What causes PCOS?
The cause of PCOS is multifactorial with obesity and genetics being most important factors.
A family history of irregular menses is usually present in most girls with PCOS. It is important to note that obesity causes delayed menses and not vice versa. Obesity increases insulin resistance which affects the pituitary and ovaries leading to an imbalance in estrogen:testosterone ratio. Excess fatcauses changes in pituitary hormone secretion with excess of LH (Leutinising Hormone) as compared to FSH. Fat increases the conversion of estrogen to estrone which has male hormone activity. Fat also increases the levels of active male hormones. These hormonal changes cause a delay in menses, acne and hirsutism.
Points to remember
PCOS cannot be cured. The features can be treated and monitored but will relapse once your efforts slacken.
Weight gain worsens PCOS, so exercises and diet care need to be continued on a long term basis.
Gestational diabetes Mellitus
What is Gestational Diabetes Mellitus?
The incidence of diabetes in pregnant women worldwide is 3-10 per cent. Gestational Diabetes Mellitus (GDM) refers to diabetes with onset or first detection in pregnancy. It is the effect of pregnancy hormones which increase insulin resistance and blood glucose levels.
What are the probable causes?
Obesity, age at conception, family history, ethnicity (Asian race) , PCOS, history of delivering a big baby in the past or high blood glucose in the past increase the risk of diabetes in pregnancy.
Will the presence of diabetes affect the baby in womb?
Diabetes in pregnancy increases the risk of heart, neurological, kidney, intestinal and spine malformations. Maternal diabetes increases risk of poly/oligohydramnios (excess or insufficient water in uterus), hypertension and placental insufficiency. This can lead to foetal growth retardation, birth trauma, abortion and rarely foetal deaths. Babies born to diabetic women can have macrosomia (birth weight >4.5 kgs), higher rates of respiratory distress, jaundice and infections needing intensive care management.
Will the new born baby be diabetic by birth?
No. Babies born to diabetic women have low blood glucose (and not diabetes) at birth. Rarely babies can develop diabetes in infancy. This is usually because of genetic mutations and is unrelated to maternal diabetes. However, babies born to women with GDM have higher risk of obesity and Type 2 Diabetes later in life.
Can a diabetic mother undergo a normal delivery?
Yes, a diabetic mother can undergo a normal delivery provided her diabetes is well controlled and the mother and baby have no complications. However, uncontrolled diabetes, foetal macrosomia, maternal complications like hypertension and obesity, twin pregnancies, breech or transverse presentations, past miscarriages or still births necessitate caesarean sections.
Conclusion:
If a diabetic mother is careful with her diet, exercises, blood glucose monitoring, medications and follow-ups, there is no need to fear and she can deliver a healthy baby
 Back to Site
Back to Site