Hypertensive emergencies (formerly called malignant hypertension) encompass a gamut of clinical presentations in which uncontrolled blood pressures (BPs) lead to progressive or impending end-organ dysfunction. In these conditions,the BP should be lowered aggressively over minutes to hours. The presence of acute and rapidly evolving end-organ damage with an elevated diastolic blood pressure,usually greater than 120 mmHg, establishes a diagnosis of hypertensive emergency.
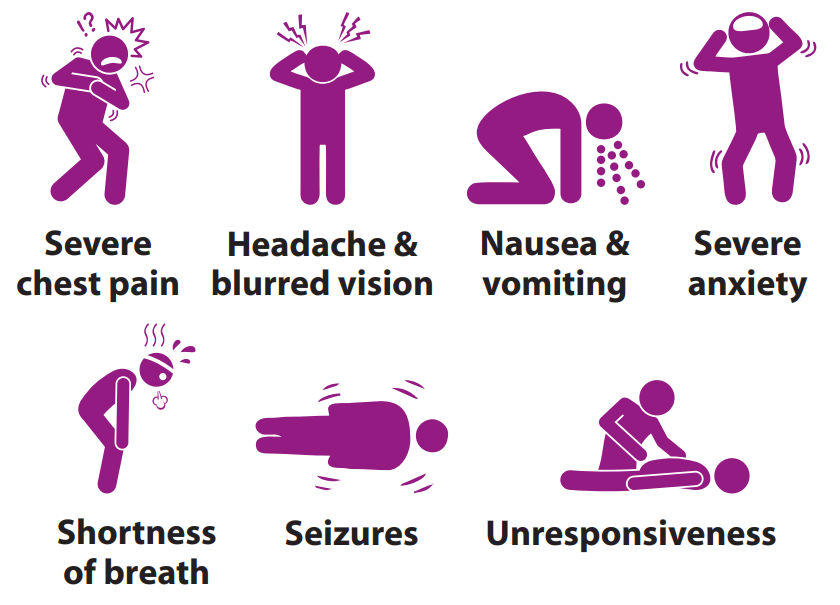
Signs and symptoms of a hypertensive emergency
The most common clinical presentations of hypertensive emergencies are cerebral infarction (24.5%),pulmonary oedema (22.5%),hypertensive encephalopathy (16.3%), and congestive heart failure (12%). Other clinical presentations associated with hypertensive emergencies include intracranial haemorrhage, aortic dissection, and eclampsia, as well as acute myocardial infarction.
Multidisciplinary approach
Hypertensive emergency requires a multidisciplinary approach.Cardiac concerns may invite other ailments related to different organs of the body. A thorough clinical examination and investigation can direct the treatment with involvement of appropriate specialists.Our multidisciplinary team includes cardiologists,neurologists, nephrologists, cardiac surgeons, neurosurgeons and interventional radiologists, who get involved in the treatment process based on presentation of the disease.
Look for these End-organ damages
- Neurologic end-organ damage
due to uncontrolled BP may include hypertensive encephalopathy, cerebral vascular accident/cerebral infarction, subarachnoid haemorrhage, &/or intracranial haemorrhage. - Cardiovascular end-organ damage
may include myocardial ischemia /infarction, acute left ventricular dysfunction, acute pulmonary oedema, &/or aortic dissection. - Other organ systems
may also be affected by uncontrolled hypertension, which may lead to acute renal failure/insufficiency, retinopathy, eclampsia , or micro angiopathic haemolytic anaemia.
Patients may complain of specific symptoms that suggest end-organ dysfunction
- Chest pain may indicate myocardial ischemia or infarction
- Back pain may denote aortic dissection
- Dyspnoea may suggest pulmonary oedema or congestive heart failure
- The presence of neurologic symptoms may include seizures, visual disturbances,and altered level of consciousness and may be indicative of hyper tensive encephalopathy
How to treat
Hypertensive emergencies are treated in an ICU.Blood pressure is progressively (although not abruptly) reduced using a short-acting, titratable IV drug.Choice of drug and speed and degree of reduction vary somewhat with the target organ involved,but generally a 20 to 25 per cent reduction in MAP over an hour or so is appropriate, with further titration based on symptoms.Achieving “normal” BP urgently is not necessary. Typical first-line drugs include Nitroprusside , Enalaprilate, Nitroglycerine and Labetalol etc.
Hypertensive emergency requires multidisciplinary team approach and referral to the respective team depending upon end – organ involvement.
 Back to Site
Back to Site