MRI has taken leaps and bounds with advances in applications since its inception in clinical practice in late 1980s and early 1990s. Neuroradiology has always been at the forefront of research applications and most of the advances in MRI have been in this speciality. The basic anatomical MRI images still form the core of the study which evaluates brain morphology and structure, the newer sequences and advances now give us information and insight into brain function. With current advances, there is further invaluable support for many clinical situations such as tumour surgery, epilepsy surgery, hemodynamic and differentiation between various brain pathologies.
Some of the techniques that are used with the clinical applications are outlined below.
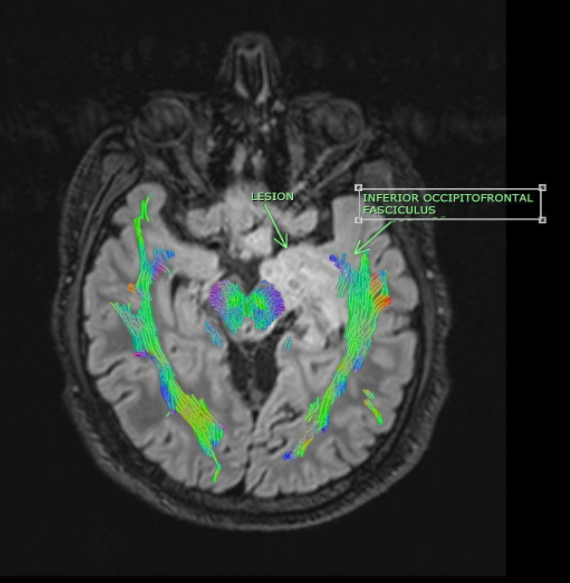
Diffusion Tensor Imaging (DTI)
A specialized MRI brain or spinal cord that evaluates neural pathways within the brain, brainstem, or spine, such as motor controls and speech. Currently it is an adjunct to a routine MRI brain. DTI is the process to map out white-matter fibres which may be able to show something is abnormal where the fibres are or are not well-organized. We use this technique prior to all brain tumour and epilepsy surgeries for infiltration and avoiding injury white matter tracts. It helps neurosurgeons recognise parts of the eloquent tracts of the brain which should not be touched during surgery.
Improvements in diffusion tensor imaging have enabled radiologists to understand disease processes. In short, DTI uses the diffusion of water within the neurons as a probe to determine the anatomy of a brain network, which basically provides information on static anatomy that is not influenced by brain functions.
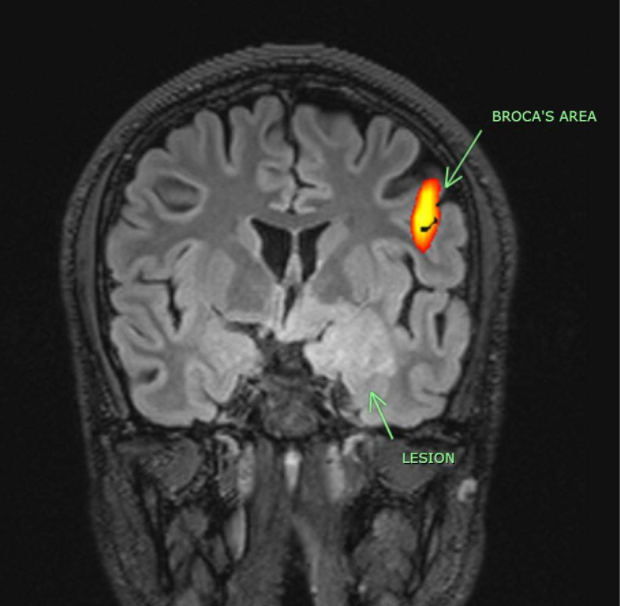
fMRI (Functional MRI)
Functional magnetic resonance imaging (fMRI) is a non-invasive and safe technique to measure and map the activities of the brain during normal as well as diseased conditions. It measures the changes in the brain’s blood flow that happen with brain activity.
The change in fMRI signal according to altered brain activity is an indirect effect, which depends on the change in cerebral blood flow caused by altered neural activity. An increased neural activity elevates the level of blood oxygenation because of an increased energy demand that subsequently calls for more oxygen. When more blood reaches the area of the brain, the signal is stronger and vice versa. This phenomenon forms the basis of blood oxygenation level-dependent (BOLD) fMRI.
We use this primarily to map eloquent areas in the brain such as the motor, sensory, language, visual cortex. This ensures the surgeon knows the exact area to be careful while operating. This is important as there could be a shift of the eloquent area in the brain due to tumour or disease, a phenomenon known as “Brain Plasticity”. Again, this enables a surgeon to be more liberal or careful during surgery.
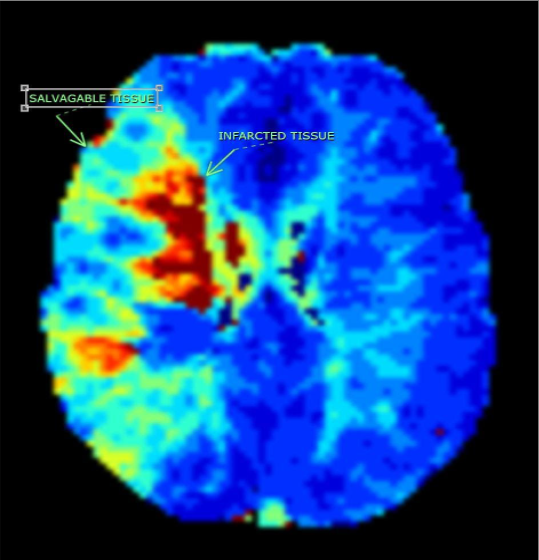
MR Perfusion
Perfusion MRI is tool to assess brain hemodynamic and microcirculatory changes in the brain non-invasively and can be used for physiologic and pathophysiologic parameters. It has been a promising tool in assessing stroke, brain tumours and patients with various vascular diseases. It can be done with and without MRI contrast agents injected intravenously. The data acquired is assessed qualitatively and quantitatively, which means we could get a general idea of regional blood flow in the brain or quantify the differences in brain blood in various regions. The different data we get is cerebral blood flow, cerebral blood volume, mean transit tine and time to peak. Each of these parameters gives us variable information to make important clinical decisions.
The mainstay of perfusion utility is stroke whereby we are able to assess infarcted tissue and separate it from the tissue at risk or the salvageable tissue. This guides us in making important treatment decisions, choosing the best treatment options and finally saves the patient from progressive neurological deficit and goes a long way improving the quality of life. In tumours, we are able to tentatively differentiate high and low grade tumours and evaluate regions of tumour infiltration for maximum safe resection.
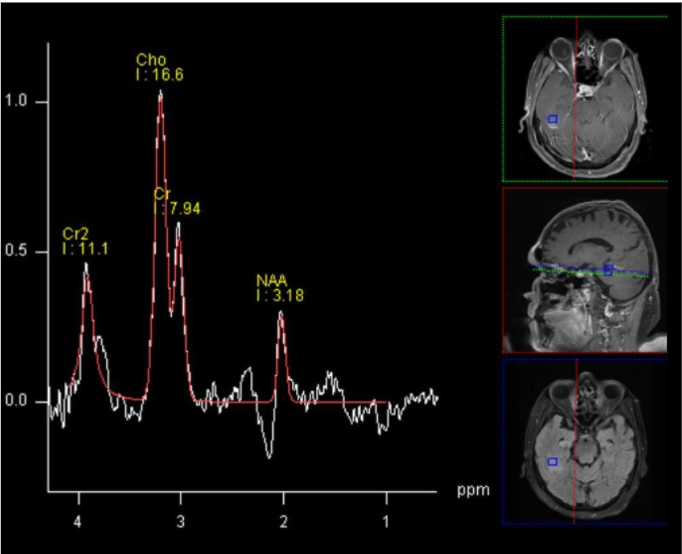
MR Spectroscopy
Magnetic resonance (MR) spectroscopy is a non-invasive diagnostic test for measuring biochemical changes in the brain, especially the presence of tumours and pediatric metabolic. It is used as a ‘case to case’ basis. While magnetic resonance imaging (MRI) identifies the anatomical location of a tumor, MR spectroscopy compares the chemical composition of normal brain tissue with abnormal tumor tissue. It is generally used to determine if a lesions tumor or not, but has to be used with other routine MRI data and should not be used as an isolated tool.
MR spectroscopy utilizes the inherent molecules in the cells, most common being hydrogen ions or protons due to its abundance. Proton spectroscopy is most commonly used. There are several different metabolites, or products of metabolism, that can be measured to differentiate between tumor or metabolic diseases such as N-acetyl aspartate (marker of neurons), amino acids (metabolic diseases), Lipid- Lactate (tissue breakdown and anaerobic metabolism, Choline (cell turnover and hence useful in tumour evaluation)
Summary
Above are some of the valuable and interesting MRI techniques that we use today. It is important to recognise that these are not standalone techniques, but used as an adjunct to ‘morphological’ or anatomical MRI images.
 Back to Site
Back to Site