Introduction
Epilepsy surgery as a treatment option is considered for patients with medically refractory epilepsy.
Medically refractory epilepsy constitutes about 20-30% of all epilepsies. The definition of medically refractory epilepsy has evolved over time. Typically, an epilepsy where 2 ‘appropriate’ anti-epileptic medications have failed to control it is considered medically refractory. It is a devastating ‘disease’. It is typically a constellation of symptoms which include uncontrolled seizures with or without status epilepticus but also cognitive decline. This disease burden, amongst other challenges also invariably leads to poor psychosocial integration. The etiology is quite varied ranging from genetic to malformations to acquired brain injury.
A subset of patients with medically refractory epilepsy have surgically remediable epilepsy. This subset needs to be identified by treating clinician – sometimes it is a plain clinical decision and at other times needs evaluation often referred to as presurgical evaluation. It is an ILAE/ AAN recommendation that every patient with surgically remediable epilepsy should be offered surgery at failure of 2nd antiepileptic medicine.
What is epilepsy surgery?
Epilepsy surgery is a mature concept. The first epilepsy surgery was performed by Victor Horsley in the 1880s- before the advent of EEG and imaging techniques.
Epilepsy surgery is a functional neurosurgery- often very different from other brain surgeries. It can be curative or palliative. It may not be a lesional resection as it aims to resect the epileptic network. The epileptic network often may not be readily identifiable. The process of identifying the epileptic network in context of functional neuroanatomy is crucial. The actual surgery is a final culmination of this process.
Presurgical Evaluation:
The process of identifying a surgically remediable epilepsy and the epileptic network in a given patient is called presurgical evaluation. This is anchored by the epileptologist. Each evaluation does not culminate into surgery.
Video EEG and MRI Brain are the cornerstones of presurgical evaluation.
Video EEG, also called as video telemetry, records seizures as well as interictal EEG in sleep and awake. This provides very useful data for starting to understand the epileptic network. MRI brain provides much needed structural information- uncovers gliosis, cortical malformations etc.
Often these 2 tests provide necessary information. In some patients additional tests are needed. MRI tractography, functional MRI (speech and motor), SPECT brain (ictal and interictal) and PET Brain are needed for some patients. Clinical neuropsychology evaluation is important for all patients undergoing epilepsy surgery. It gives a lot of valuable information regarding cognitive skills, concentration etc as well as dominance between the 2 hemispheres and lobar dysfunction.
Types of epilepsy surgery:
- Focal Resection
- Temporal Lobe Resection
- Extratemporal Resection (frontal, parietal, and occipital)
- Lesionectomy
- Multiple Subpial Transections
- Laser Interstitial Thermal Therapy
- Anatomical or Functional Hemispherectomy and Hemispherotomy
- Corpus Callosotomy
- Stereotactic Radiosurgery
- Neurostimulation Device Implantations, including
- Vagus Nerve Stimulation (VNS)
- Responsive Neurostimulation (RNS)
- Deep Brain Stimulation (DBS)
We shall illustrate this concept of curative epilepsy surgery with a case.
History:
An 8 ½ year old boy presented to us with history of seizures since six years of age. The seizures were very frequent despite adequate antiepileptic medications- 3 to 5 episodes every week in sleep in clusters. The semiology of the seizure was that he would wake up from sleep and report that he is feeling some vibrations in his right upper limb. Thereafter the seizure would progress to a right upper limb clonic seizure. Rarely he would experience a secondary generalised tonic clonic seizure. Past medical history, birth history and milestones were normal. He was attending a mainstream school and doing well. He had forced right handedness. Neurological and developmental examination was normal.
Clinical syndrome: medically refractory focal sensorimotor epilepsy.
He underwent a pre surgical evaluation as this was thought to be surgically remediable epilepsy. Results:
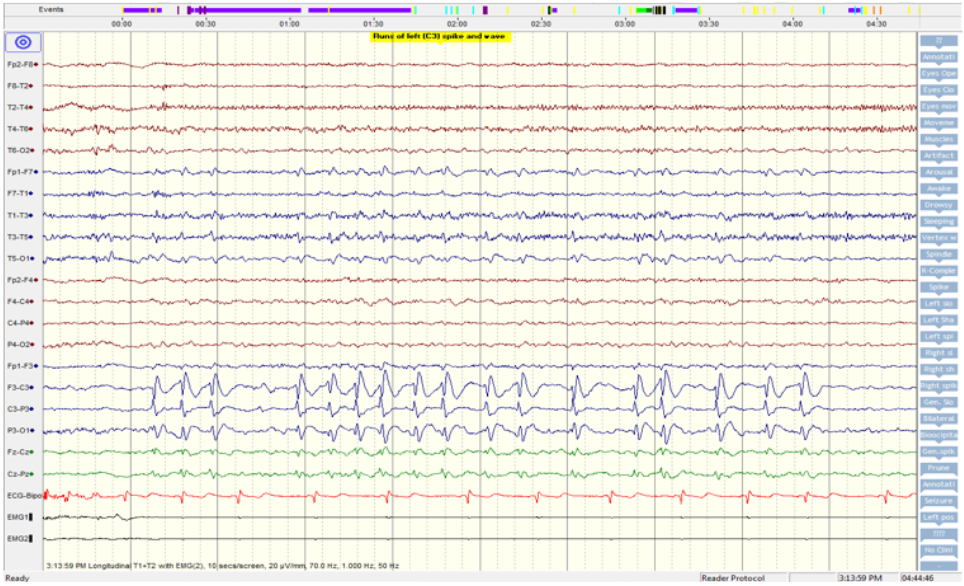
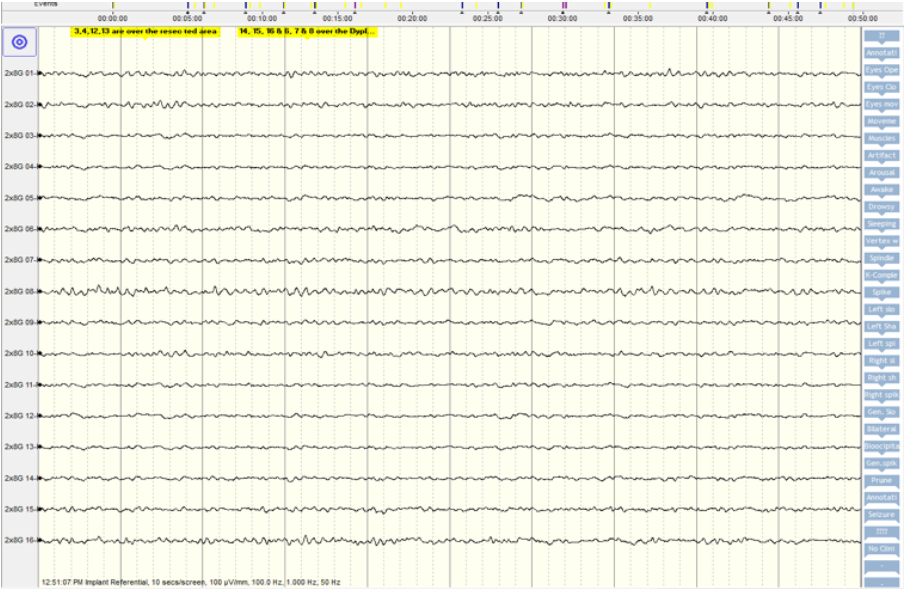
- 48 hour video EEG showed very frequent interictal abnormalities over the left frontocentral region (Figure 1). We recorded stereotypical seizures which also localised to the left motor region.
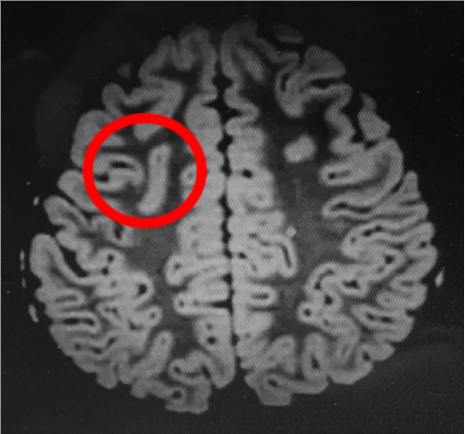
- MRI brain showed a focal cortical dysplasia over the left precentral gyrus (Figure 2).
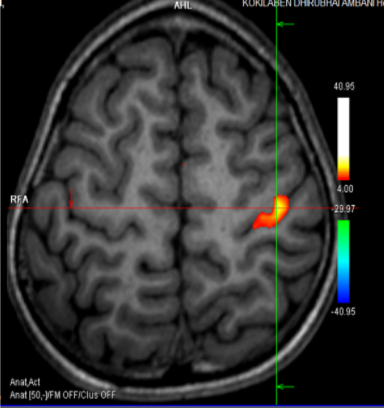
- Motor functional MRI unfortunately localised the motor function of right hand over the dysplastic precentral gyrus (Figure 3).
Hence, though surgically remediable, epilepsy surgery was not advised as it would invariably cause a right-sided hemiparesis.
1 year on,
His seizures continued unabated. He also developed academic difficulties. His grades dropped- he started failing. Also his left hand usage increased- note he was forced right handed. He started using his left hand for writing. Parents also noticed that he had developed a right-sided weakness -he could not lift his school bag with his right hand. He could not stand or hop on his right leg. So the clinical syndrome had now evolved from being a medically refractory epilepsy to that of an epileptic encephalopathy with motor and cognitive regression.
We revisited his presurgical evaluation-the Video Eeg and functional MRI were essentially unchanged. However it became more and more clear that he had a sensory aura before the motor manifestations in the seizure. Options for surgery were 2 stage or an awake surgery: to check eloquence. However neither of these were thought to be feasible by the parents and the team. Hence we decided to go ahead with focal cortical dysplasia- guided by electrocorticography, motor evoked potentials with cortical stimulation and intra operative MRI as needed. We had discussed a strong possibility of permanent post-operative hemiparesis with the family.
Epilepsy Surgery:
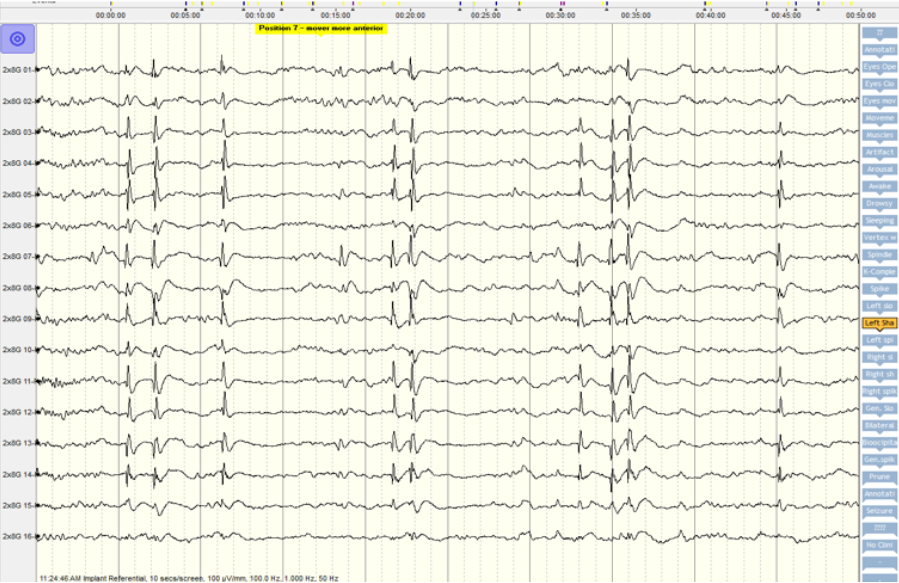
Prior to resection in the OT we had to demarcate the resection boundaries. We used neuronavigation, electrocorticography, MEPs and cortical stimulation. Electrocorticography localised the maximum epileptogenicity over the post central (not precentral) gyrus ie sensory cortex (see figure 4a). This was very well concordant with the clinical semiology. Hence we resected only the postcentral gyrus. After this resection a repeat electrocorticography showed NO epileptic discharges (see figure 4b). We did not resect the dysplasia overlying the precentral gyrus.
Follow up:
He has no neuro deficits. His cognition has improved back to baseline and he is doing well in school. He has started writing again with his right hand. He has had no seizures since the surgery in 2016. We have continued one antiepileptic medication in view of the residual focal cortical dysplasia as well as minor abnormalities on his EEG.
 Back to Site
Back to Site