It has been over five decades that the pioneering Indian Neurosurgeons introduced the specialty to the masses. Owing to the morbid nature of the neurosurgical disorders and the sequela of treatments there has been an innate stigma associated with neurological surgery in the medical fraternity and the populace. With emergence of better radiological techniques, early and accurate diagnosis of brain tumors has been possible demanding a prompt and precise treatment. There has also been a paradigm shift in the primary goals of neurosurgical oncology. It has changed from diagnosis, prognostication and palliation to achieving longevity with superior quality of life. The cornerstone of achieving this outcome is maximal tumor resection with preservation of the functional cortical and subcortical tissue.
Knowing of the location of these functional areas in relation to the tumor is important during the surgery. Neurosurgeons employ various radiological, electrophysiological and navigational tools to achieve this. One method to achieve this is to perform the surgery awake with use of intraoperative neurophysiological monitoring and constantly test the patient’s brain function. However, owing to the distortion of brain around the tumor the technique of identifying the functional areas in an awake patient would prove akin to finding needle in the haystack.
This daunting task would be made much easier if we can have a map to the brain before we start navigating through it during the surgery. The conventional MRI gives us structural information of the brain-tumor tissues, blood vessels and fluid spaces in and around it. The use of functional MRI (fMRI) adds an additional layer of information. This identifies the cortical areas (areas on surface of brain) critical to the functions such as hand and leg movement, language, vision etc. Then there are fiber pathways that interconnect these functional areas with each other and with rest of the body. The entire substance of brain (white matter) is crisscrossed with these fibres. Preserving these “information highways” is equally important to safeguard the functional integrity of the body. The technique of identifying these subcortical (under the surface of the brain) fiber tracts is called as tractography. Utilization of all this preoperative information along with awake intraoperative monitoring to carry out the brain tumor surgery helps to make the procedure a safe and successful enterprise. (VIDEO 1)
The science behind diffusion tractography is deterministic evaluation of anisotropic movement of water molecules along the subcortical white matter fibres. With help of this technique we can identify the fibres connecting brain with hands and legs (cortico-spinal tracts), language areas with each other (dorsal and ventral language streams), eyes to the brain (optic tracts). The information of these fibres with relation to the brain tumor is known. It also tells us if the fibres are shifted, distorted or invaded by the tumor or the surrounding edema. Additionally, the location of these fibres can be confirmed intraoperatively using navigation and sub-cortical electrical stimulation. A successful tumor resection would require to preservation of these functional sub-cortical white matter tracts while achieving maximal safe resection of the tumor.
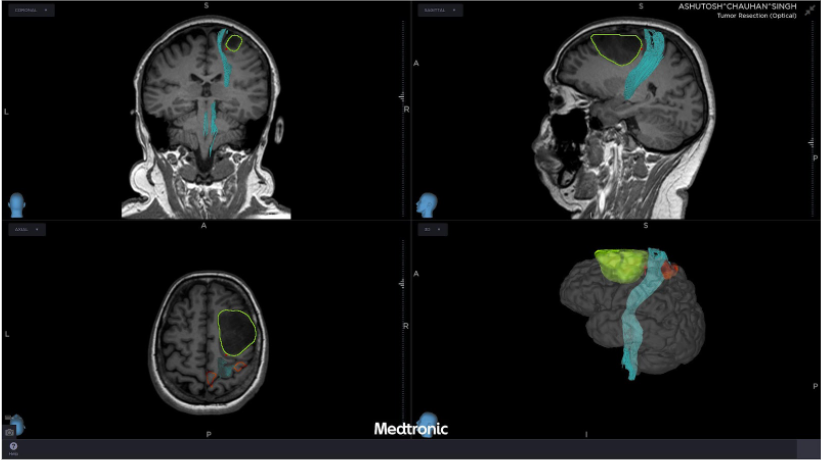
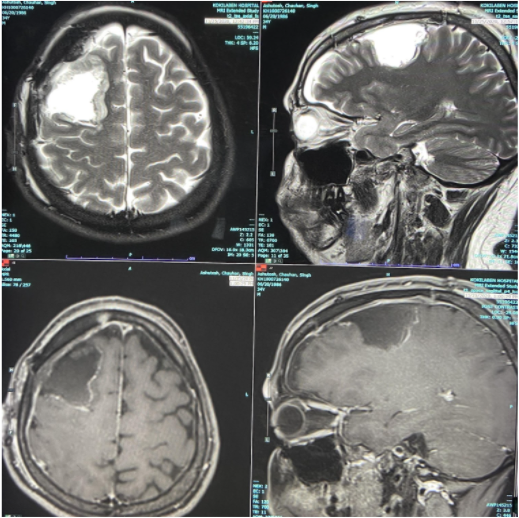
Illustrated Case: 47 years male, presented with seizures and right frontal tumor displacing the cortico-spinal tract posterio-medially (FIGURE 1). Awake surgery with intraoperative monitoring helped in successful complete tumor resection with identification and preservation of the motor fibres. (VIDEO 2, FIGURE 2).
Tractography is a robust tool to help plan and execute complex brain tumor surgery. Its utilization along with other intraoperative tools makes the brain surgery safer and ensures high degree of function preservation. Inclusion of this technology has made achievement of complete/ maximal safe tumor resection with prolonging the patient life a reality.
APPENDIX
Left Parafalcine Glioma. Green Segmentation: Tumor; Orange Segmentation (BOLD Signal) clockwise: fMRI (Supplementary Motor Area, Hand Area, Leg Area, Wernicke’s Area, Broca’s Area);
White Matter Tracts: Pink- Frontal Aslant Tract, Light Blue – Motor Fibres, Ochre – Middle Longitudinal Fasciculus, Yellow-Arcuate Fasciculus, Orange – Inferior Fronto-Occipital Fasciculus, Dark Blue – Uncinate Fasciculus, Red – Inferior Longitudinal Fasciculus
 Back to Site
Back to Site