Stroke due to Carotid Stenosis – treatment by carotid stenting
Carotid artery stenosis is one of the most common causes of ischemic stroke. Conventionally, CAD was treated by CEA till late; however, the emergence of interventional neuroradiology has revolutionized the treatment of the disease with endovascular surgery in the form of carotid stenting. We present a case of a 60 yr old female detected with acute stroke due to severe narrowing of carotid lumen that was treated successfully with carotid artery stenting.
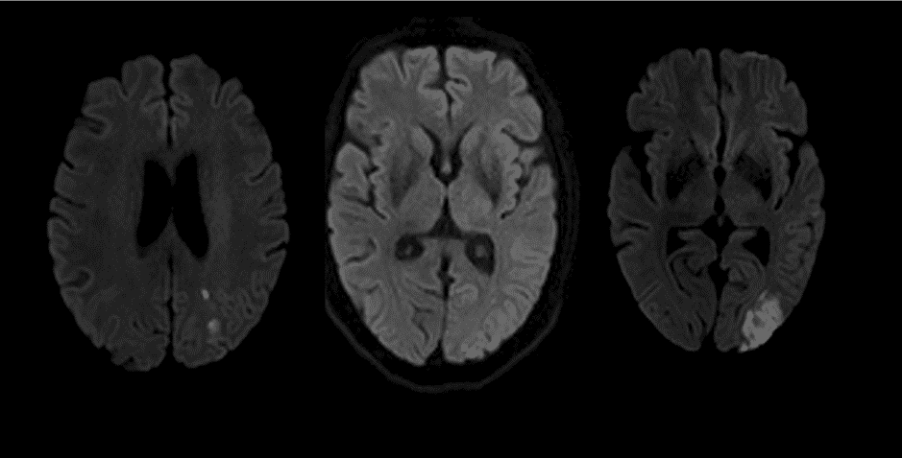
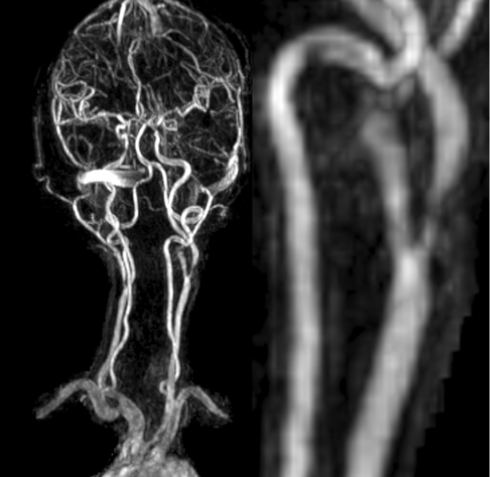
A 60 year old right handed Indian housewife with past medical history of hypertension, diabetes mellitus & hyperlipidemia was brought to emergency for fluctuating right sided weakness & slurring of speech over a period of 4 hours. The presenting National Institutes of Health Stroke Scale (NIHSS) score was 4. MRI of the brain & angiography demonstrated acute non-hemorrhagic left MCA territory infarcts involving posterior parietal lobe and severe stenosis of the left carotid bulb. (Fig 1, 2)
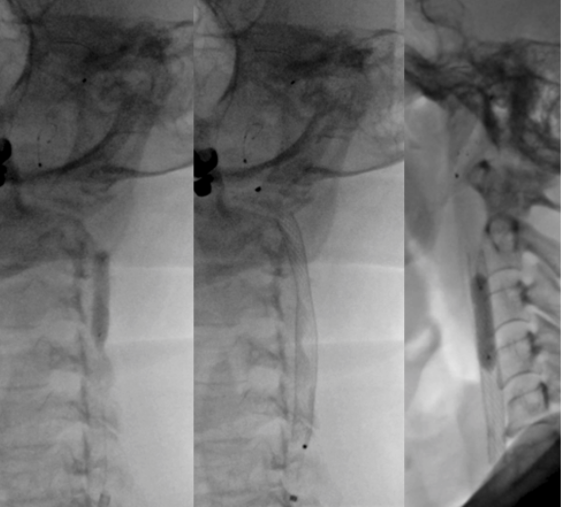
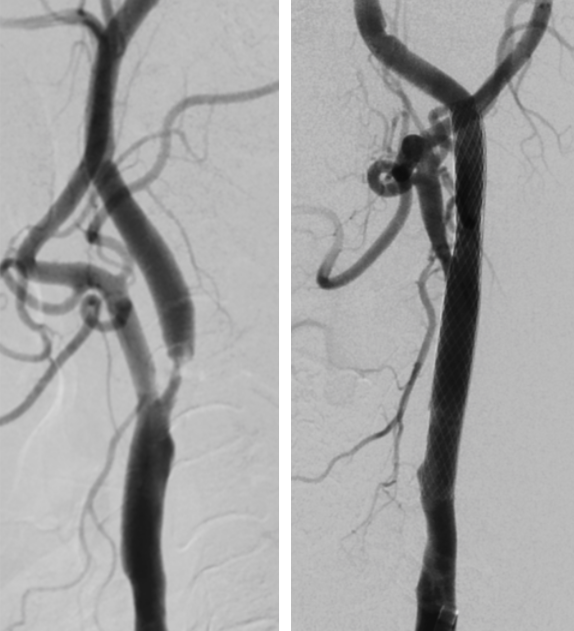
The patient was administered 450 mg of Clopidogrel & 300 mg of Ecosprin. Diagnostic angiography was performed with 5 Fr H1 (CORDIS, Santaclara, California, USA) catheter. Left common carotid injection confirmed high grade stenosis (approx. 90%) (Fig 3). Stenting was planned under local anaesthesia and an 8 fr sheath was placed in the right femoral artery followed by guiding catheter was navigated into the left common carotid artery. A distal protection device (7 mm spider) (Medtronic, DUBLIN, IRELAND) was placed under roadmap guidance into the distal cervical internal carotid artery. The pre-plasty was done with 5 X 20 mm Viatrac balloon (Fig 4a) (ABBOTT, Chicago, Illinois, USA). The self expanding closed cell design Wall stent 9 x 40 mm (Fig 4b) (BOSTON SCIENTIFIC, Marlborough, Massachusetts, USA) was carefully deployed across the maximal stenosis. Post stenting angiogram revealed moderate waist at the site of stenotic lesion which was dilated by 5 X 20 mm Viatrac balloon (Fig 4c) (ABBOTT, Chicago, Illinois, USA). Post stenting angiogram shows brisk flow across the stent with good recanalization of the stenotic segment followed by which distal protection device was removed (Fig5).
Patient tolerated the procedure well with an uneventful post-procedure stay. She was discharged 2 days after the procedure with paresis of the right upper extremity. She had an NIHSS score of 1 & modified Rankin Scale score of 1.
The development of atherosclerotic plaque at the carotid bulb leads to luminal stenosis. AHA report published in 2012 suggests that 25% cases of ischemic stroke are caused by carotid artery stenosis (1).
Carotid artery stenosis can be diagnosed with ultrasound doppler, CT Angiography (CTA) or MR Angiography (MRA), limiting the use of traditional catheter angiography as a precursor to endovascular treatment. The treatment of carotid stenosis has been surgical over the course of decades. With various trials being conducted in late 90s on both asymptomatic and symptomatic patients (2,3,4). ACAS trial of 1995 concluded that endarterectomy in patients with asymptomatic carotid narrowing of greater than 60 percent have a reduced 5-year risk of ipsilateral stroke given that the surgery was performed with less than 3% peri operative morbidity and mortality. NASCET and ECST trials favoured endarterectomy in patients with recent history of non disabling ischaemic events and in patients with moderate however symptomatic stenosis of 50-69%.
The Consensus over when one should undergo intervention for stenosis i.e, >50% narrowing in symptomatic CS and >60% in asymptomatic CS, remains the same. Recent introduction of carotid artery stenting has changed the traditional approach of treatment of the disease. Various studies have sought to compare the outcomes of CEA and CAS over the tenure of the last 10 years. An ICSS study of 2015 conducted on 1710 patients showed a 5 yr disabling risk of 6.4% vs 6.5% in stenting vs endarterectomy (5). With the use of distal protection devices, stenting has become safer, as a study has shown a four-fold increase in risk stroke without the device(6). A breakthrough study published in 2017 called asymptomatic carotid trial – 2 (ACST 2) that evaluated pre procedural and post-procedural risks in CAS and CEA to be equal (7). contrasting a few earlier studies stating a minor increase in the risk of non disabling stroke in CAS as compared to CEA. The article also finds the 5 yr risk of procedural death or disabling or fatal stroke to be 3.5% and 3.4% in CEA and CAS respectively.
Similarly Large review study with four clinical trials involving 4074 patients published in Lancet Neurology in the yr.2019 showed annual rates of ipsilateral stroke per person-year to be similar for patients treated with CAS and CEA (8). A meta analysis of studies conducted on patients undergoing endovascular thrombectomy showed a favorable outcome of stenting done simultaneously with thrombectomy with reduced mRS score post procedure (9)
The cost of treatment for CAS and CES including long term hospital stay and post procedure or surgical care have been found to be almost equivalent and hence must not affect the choice of treatment for CS(10). Thus treatment of Carotid stenosis largely depends on expertise, infrastructure and local experience.

 Back to Site
Back to Site