Introduction
In the pandemic, Arterial Ischemic Stroke is now well recognised as a presenting feature or a complication of Covid-19 in adults. An acute paediatric stroke is a rare and often an under recognised medical emergency.
We report a case of a young girl who presented with a recurrence of arterial ischemic stroke in the context of her being SARS-CoV-2 PCR positive.
Case report
A 15-year old girl had presented in January 2020 with acute dense right hemiparesis and global aphasia secondary to an acute left MCA territory infarct. She had undergone mechanical thrombectomy for the same.
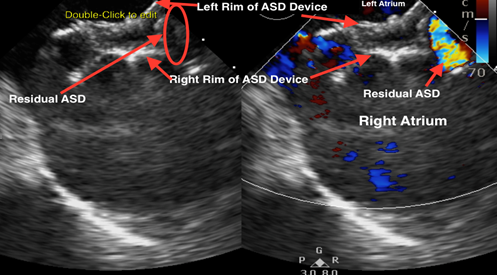
She had undergone n ostium secundum atrial septal defect device closure in 2017. A transoesophageal ECHO cardiogram revealed a residual defect in retroaortic area with left to right shunt, mild tricuspid and mitral regurgitation and normal biventricular function (figure 1). The detailed prothrombotic workup was normal. She was receiving treatment doses of low molecular weight heparin. She had accidentally never started the prescribed oral aspirin. She had improved- residual mild weakness in the right hand and expressive aphasia.
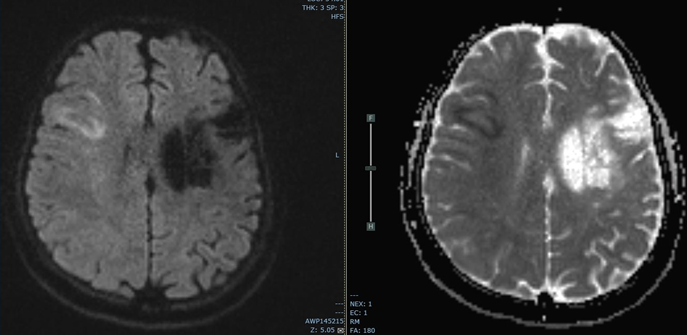
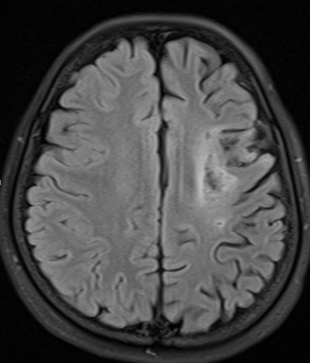
In July 2020 she presented to the emergency department for new onset weakness on the left side of her face. Examination showed left facial weakness with no other significant new neurological deficit. Ped NIHSS for the new deficit was 3. An urgent MRI brain stroke protocol showed diffusion restricted acute cortical–
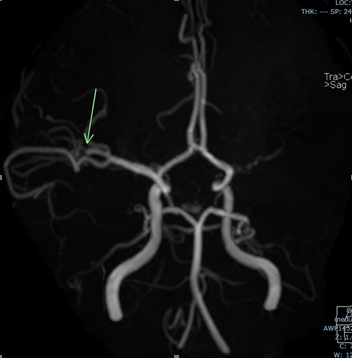
subcortical right MCA territory infarct in the frontal lobe; the MR angiogram showed focal partial occlusion of the superior division of the right MCA (figures 2, 3, 4).
We treated her with IV thrombolysis despite the low Ped NIHSS score – a case specific decision- given the underlying residual neurological deficit and a strong possibility of this being a recurrent cardioembolic stroke. The left facial weakness resolved post thrombolysis – PedNIHSS 0 for new deficit.
In the meanwhile, she tested positive by nasopharyngeal swab Xpert Xpress RT PCR assay for SARS-CoV-2. Shad had no respiratory symptoms or fever in recent past. Typical COVID-19 related inflammatory markers were normal (appendix 1). SARS- CoV2 antibody test showed a high level of Covid -19 antibodies.
No new thrombus or vegetation was seen on 2D Echo.
Enoxaparin and Aspirin were recommenced 24 hours of thrombolysis – therapeutic levels achieved of anti Xa. In 4 days. She was discharged with continued anticoagulation and ongoing neurorehabilitation for previous right sided weakness with aphasia. Since then, she has undergone uneventful cardiac surgery for device removal and an intracardiac repair of the defect.

Discussion
In paediatrics, neurological symptoms seen in the case series of PIMS-C (Paediatric Multisystem Inflammatory Syndrome temporally associated with COVID-19) 13 have been encephalopathy, brainstem and cerebellar signs, headaches, muscle weakness and reduced reflexes with splenial changes on MRI, slowing on EEG and mild abnormalities in EMG-NCS.
There are just two, isolated case reports of strokes in children with Covid -19 – primarily with focal cerebral arteriopathy.15
There is an etiological conundrum in our case. Our patient tested positive in her nasal swab for SARS CoV-2 by PCR with simultaneous high titres of anti-SARS CoV-2 antibodies. Her inflammatory markers were normal. She had a pre-existing risk factor – left to right small residual shunt across the ASD device. However, she was receiving effective doses of LMWH.
The dilemma is what caused the recurrent thrombosis – was it purely of cardiac origin despite anticoagulation or was a prothrombotic process triggered off by a recent otherwise asymptomatic SARS-CoV-2 infection.
References
Evolutionary history, potential intermediate animal host, and cross-species analyses of SARS-CoV-2 Li X et al J.
- Med. Virol. 2020
WHO Director-General’s opening remarks at the media - briefing on COVID-19 – 11 March 2020
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China Huang C et al Lancet. - 2020;395:497–506
Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China Mao L et al - JAMA Neurol. 2020
Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study Li Y et al - Stroke Vasc Neurol Sept 2020
Neurological manifestations in severe acute respiratory - syndrome Tsai L.K. et al Acta Neurol. Taiwan. 2005
SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor - Hoffmann M et al Cell. 2020
Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19 Steardo L et al Acta - Physiol. (Oxf.) 2020
Critically Ill COVID-19 infected patients exhibit increased clot waveform analysis parameters consistent with - hypercoagulability Tan C.W et al Am. J. Hematol. 2020
Acute pulmonary embolism and COVID-19 pneumonia: a - random association? Danzi G.B., et al Eur. Heart J. 2020
Pulmonary and cardiac pathology in Covid-19: the first autopsy series from New Orleans. Fox SE et al medRxiv - 2020
COVID-19 autopsies, Oklahoma, USA Barton L.M. et al - Am. J. Clin. Pathol. 2020
Neurologic and Radiographic Findings Associated With COVID-19 Infection in Children Omar Abdel-Mannan et - al JAMA Neurol 2020
Neurological Manifestations of COVID-19: A systematic review and current update A. Whittaker et al Acta Neurol - Scand. 2020
Vessel Wall Enhancement and Focal Cerebral Arteriopathy in a Pediatric Patient with Acute Infarct and - COVID-19 Infection E. Gulko, et al AJNR Aug 2020
 Back to Site
Back to Site