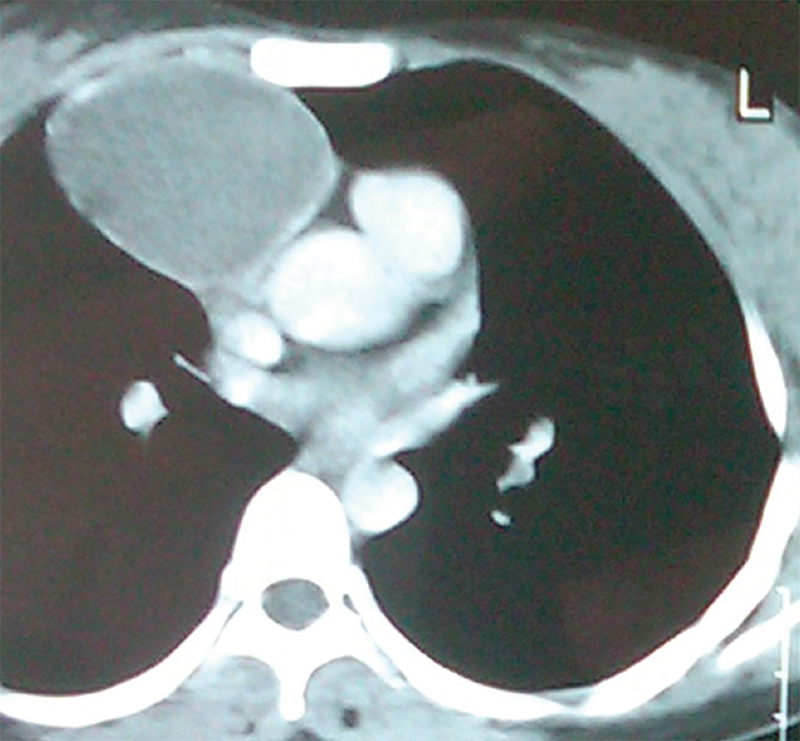
PS, a young 25 year-old woman, came to us with chest pain that she had been suffering from for four months. Clinical examination was unremarkable. Imaging of the chest revealed a moderatesized superior mediastinal mass abutting the major vessels without any infi ltration of mediastinal structures (fi g 1). CT guided Fine Needle Aspiration Cytology (FNAC), performed prior to reporting to KDAH, revealed acellular fluid.
Differential diagnosis included tuberculous lymphnode or teratoma. After relevant investigations, she was taken up for thoracoscopic excision of the mediastinal mass. The patient was given general anesthesia with double lumen endotracheal tube. Her right lung was collapsed; the right thoracic cavity was accessed with three ports (one for telescope (10 mm) and two (5 mm) for instrumentation).

A well encapsulated mass was seen in the superior mediastinum abutting the pericardium, pulmonary hilum and Superior Vena Cava (SVC). It was freed from its attachment with combination of blunt and sharp dissection. The tumour was inserted in a plastic bag after aspirating the fluid within and delivered through 10 mm port. At microscopy it was reported to be a benign mature teratoma.
DISCUSSION
The case is being presented to highlight the role of video-assisted thoracoscopic surgery (VATS) in management of thoracic tumours. Normally this tumour would have required either median sternotomy or postero-lateral thoracotomy. Both of these are known to be associated with signifi cant post-operative pain leading to reduced cough and breathing effort resulting in pulmonary morbidity. VATS does not involve a large incision, cutting of muscle or bone, hence it is cosmetically more acceptable to patients; it results in faster and relatively painless recovery (fi g 2). VATS is an accepted technique for surgical management of several thoracic tumours in properly selected cases and high volume centres.
 Back to Site
Back to Site